AORN Congress # 48 in Dallas, TX, March 11-15, 2001
5276 RNs and 5713 exhibitors (as of March 14 at noon) for a total of 10, 989

In a similar vein, delegates also passed the "Resolution on Responsibility for Mentoring." This resolution was not only directed towards mentoring students, but also directs the perioperative nurse to seek opportunities to mentor other persons interested in exploring perioperative nursing as a career, novice periop nurses, inexperienced periop nurse managers, and emerging leaders. The resolution states that the perioperative nurse mentor will model professional behavior and demonstrate a commitment to periop nursing by participating in professional organizations, supporting practice-related legislative and regulatory initiatives, and by maintaining an awareness of international health care issues affecting the practice of perioperative nursing.
Our Delegate Chairman, Sophie Taylor, gave me on of my best Congress "assignments" ever – the two (2) foci of my report to you are related to perioperative nursing research and our association’s bylaws.
It didn’t seem as if there were as many research posters this year as there have been in the prior Congresses. The one I am choosing to present to you is titled The Effects of Intraoperative Warming Therapy on the Incidence of Postoperative Pressure Ulcers and Wound Infections: A Randomized Clinical Trial. " The two (2) English nurse researchers who conducted this study looked at 338 patients selected at random. Their main hypothesis was that keeping patients warm during surgery would reduce the incidence of postoperative pressure ulcers. Previous research has shown that maintaining normothermia reduces the incidence of surgical wound infection. A secondary outcome of this study was to validate this finding.
Patients in this study were those having orthopedic, general abdominal, vascular and urological surgical procedures. A forced air warming blanket was used on half of the patients while the control group received standard care with no warming devices of any type used.
I felt that the results were very significant. Pressure ulcers in the warmed patients were reduced by 46% as compared to those receiving standard care. I expected this study to further confirm that warming patients did decrease the incidence of infection, and it did, however I was very surprised that these researchers found an incredible 88% relative risk reduction!
Given the fact that pressure ulcers incur an annual estimated cost of $3.6 billion in the United States, this study reinforces the importance of using warming blankets on all of our patients preoperatively, intraoperatively and postoperatively.
As you all know, the AORN Board of Directors developed a proposal to add an additional membership category to the existing bylaws. The Board felt this addition would create a category for individuals who support the mission of AORN and who are primarily engaged in one of the following professions: health care industry representative, central service professional, physician, health care administrator, or pharmacist.
In the first forum, a suggestion was made to change the word affiliate to the word associate. I supported this change because the definition of associate (joined or connected together as a partner or friend) better reflected how I view the relationship.
I expected to hear more opposition than I did (perhaps we are beginning to think more with our heads instead of our hearts). Further changes were proposed and adopted at the final House of Delegates. Paragraph one of Article II, Section 3 now reads:
Categories of membership in this Association are chapter member, member at large, retired, student, and associate member.
A second paragraph to Article III, Section 3 of our national bylaws was approved. This paragraph reads:
E. Associate: An individual who supports the mission of AORN and who is primarily engaged in one of the following professions: health care industry representative, central service professional, physician, health care administrator, perioperative facility and material management, informatics personnel, or pharmacist.
1. Qualifies to be an associate member at large.
2. If a chapter membership is selected, applicable chapter dues may be assessed.
3. May not hold elective office.
4. May not serve as a delegate to the AORN House of Delegates.
5. This is a nonvoting category.
Our bylaws committee will be meeting in April to revise our chapter bylaws to reflect this change and we are hopeful that it will be brought to the membership before we adjourn for the summer months.
One of my delegate assignments was to write about a Congress poster. I selected Measurement of Critical Thinking Skills in Operating Room Nurses: Diploma vs. Associate vs. Baccalaureate . I’ve written this article several times trying to be more objective (and I failed). Let me state my biases to start: I’m a diploma graduate and have worked in the OR for 27 years. I obtained an AS degree by taking two additional college classes after my basic three year diploma nursing education. I have also taken additional classes for a BSN. Critical thinking was one of these classes. I honestly feel this class helped me in watching TV news programs and reading the newspaper and did little for me in my nursing career.
This poster presented findings in only one operating room in Tucson, AZ. There were only 30 nurses in this study. There were only four diploma nurses, 13 BSN (Baccalaureate ), and 13 AD (Associate) nurses involved. The diploma nurses were the oldest with an average age of 49 (with 9-30 years in the OR). The AD nurses had an average age of 44 (with 0.5 - 12.5 years in the OR). The BSN nurses had an average age of 44 (with 2.5 - 26 years in the OR). The California Critical Thinking test was given to all 30 nurses. The BSN nurses scored 88, AD nurses scored 76, and diploma nurses scored 77. Does this prove that BSN nurses have better critical thinking skills or are younger and have taken this test before in school whereas the older diploma nurses did not? Does this prove knowledge or test-taking skills? Is age relevant to test-taking?
Critical thinking skills in action were determined by counting the number of times a nurse left the room to obtain supplies. (I fail to understand how this can determine critical thinking skills. It seems like more of an organizational ability coupled with experience and knowledge.) The diploma nurses (all four of them) scored the lowest. Donna Benotti (another delegate and diploma grad) said the diploma nurses were obviously the oldest and were probably given the newest techs or nurses to work with due to their experience. If the scrub person was inexperienced or lazy or was simply not thorough in picking a case, then the nurse would have to leave the room a lot to get additional supplies. The diploma grads could have been given the more difficult cases or more difficult surgeons. We all have had cases where the preference sheet is worthless in that case and the surgeon wants different sutures or different instruments than listed. There was no mention of a case cart system in this OR, how well the case cart system worked, how many supplies the OR team needed to gather in the OR, who the nurses were teamed with, if the nurses helped pick cases or were busy with anesthesia, drugs, interviewing, etc. There were too many variables not addressed in this study.
The results of this study were that a critical thinking skills mix of OR nurses should be taken into consideration when hiring. With the current shortage, I have personally experienced being hired over the phone upon hearing “27 years in the OR.” Education and abilities were not questioned. A warm body with OR experience and willing to work full time was the basis for hire (I didn’t take that position).
To determine that BSN nurses have better critical thinking skills than other nurses with lower levels of formal education needs a broader, more focused study. A study of only 30 nurses in one OR with only four diploma nurses in the study is too small to be significant.
On a side note, I was sad when my diploma nursing school closed in 1977 but when it was announced March 28 that my nursing school hospital was closing after 114 years, I was heartbroken. The Genesee Hospital in Rochester, NY will close within 90 days of March 28, 2001 (www.rochesternews.com/0328genesee.html). How sad for the Rochester community and for all the nurses it educated and nurtured. I learned OR nursing at Genesee and will be eternally grateful for the wonderful foundation of OR nursing I received there (from Rosemary Roth).
AORN always has at least one motivational speaker at Congress. This year it was Keith Harrell. It seemed everyone but me was enthralled with him but apparently I have a bad attitude! My initial impression was that of a mediocre TV preacher. He was full of platitudes so I wasn’t too impressed. When he started a comedy routine, I was more accepting since the banal comments ceased for a while. In short, you get to choose your attitude, so choose a good one! So on that positive note, here are a few things that pleased me in his revival meeting presentation manner. He mentioned a quote from Charles Swindoll which I’ve included at the end of this article. He made a statement that I think is fabulous - “Worrying is a negative form of meditation.” And he related a wonderful story of when he worked for IBM (he worked for them for 14 years). There was a large gathering of 650 people when it was announced there’d be layoffs. The announcer said 80% of those 650 wouldn’t be around in three months. Keith said he raised his hand and asked if he could have a bigger office with a window. That statement was hilarious (and reflected a very positive attitude!) and everyone laughed and that humor broke the black cloud mood that had descended over that group with the layoff announcement. Keith was part of that 80% laid off but he demonstrated humor plays an important role in seemingly dark situations. While everyone was plunged into instant worry and anxiety at the announcement, he lightened the mood (at least for a minute) with his positively focused comment.
"The longer I live, the more I realize the impact of attitude on life. Attitude, to me, is more important than facts. It is more important than the past, than education, than money, than circumstances, than failures, than successes, than what other people think or say or do. It is more important than appearance, giftedness, or skill. It will make or break a company ... a church ... a home. The remarkable thing is we have a choice every day regarding the attitude we will embrace for that day. We cannot change the inevitable. The only thing we can do is play on the one string we have, and that is our attitude ... I am convinced that life is 10% what happens to me, and 90% how I react to it. And so it is with you ... we are in charge of our Attitudes."
I entered the room with the preconceived idea that I wouldn’t like anything Ralph Nader had to say and that AORN needed a PAC. I came away with the opposite viewpoint and feeling like Ralph Nader was a true motivational speaker and Joel Blackwell was in the same category with Keith Harrell (full of platitudes and no substance).
Joel Blackwell said political action committees (PACs) are there to educate and to give information to lawmakers. To do this, PACs must wine and dine (and more) the legislators. Blackwell had a superb television and stage presence. He knew how to tell a good story and had a more commanding presence than Nader. But he lacked substance. I could easily picture him glad-handing the legislators.
Ralph Nader said PACs are corrupt. They have their own culture and are based on a corrupt premise - to get to a legislator, you must give him money. This is bribery. Nader told us to contact lawmakers who have had surgery (look at the ages of the legislators - they’ve had to had prostatectomies and pacemakers!). They’ll be more sympathetic to our causes. Nurses have the highest integrity rating of any profession. That works to our advantage. Nader said grassroots organizing is better than a PAC. He suggested accessing www.citizen.org/hrg (the health research group section of his web site).
Nader said no matter how much money we raise, it’ll be small compared to other PACs. Hospital chains and physician PACs are much larger. He warned our organizational focus may change with a PAC. Campaign finance reform has started and some politicians will refuse money.
Nader said a strong grassroots effort means more than a small PAC. Contributions from individuals (identifying yourselves as members of AORN and including $25 or $30 personal checks) are much more meaningful than money from PACs (Blackwell agreed with this).
Can AORN have a lobbyist without a PAC? We could but money from a PAC is very helpful. Nader suggested having a news report with press coverage about a hot patient topic will be more effective than a PAC. No PAC can legally give more than $5000 to one candidate per election. Corporations (including AORN) can’t legally give money to candidates (since 1911). Political party contributions are different - corporations may contribute to them.
Blackwell said the rules are easy to set up a PAC. Nader said it costs $100,000 to $150,000 to set up a PAC. Administrative costs are high at the beginning of a PAC. They should be audited yearly. Most PAC funds go for television advertising. Some PACs are unsuccessful (such as the tobacco PAC recently).
As I said, I was pro PAC walking into this presentation and less than halfway through, I was an adamant supporter of the grassroots method and against PACs. AORN is to be commended for arranging for these two speakers and the superb questions that were asked. It was very educational! I recommend the tape of this presentation. It has valuable information.
There were 1264 delegates registered at the First House of Delegates and that number dropped to 1253 when voting took place on Thursday, March 15. California had the most delegates with 118. Texas was the next largest group with 97. States announce their delegate contingent like the states do at the Democratic and Republican party conventions. There are signs with the states’ names and a state reporter who takes the tally from each chapter president as to the number of delegates present. People introduce their states in humorous ways. Florida announced their delegate number and then said they had no hanging chads.
The possibility of “one member, one vote” and the end of the delegate system will be brought to the 2002 Congress. A task force will be developed to explore this.
A Governance Task Force has been established.
Associate membership was approved. An associate member is one who supports the mission of AORN and who is primarily engaged in one of the following professions: health care industry representative, central service professional, physician, health care administrator, materials manager, informatics personnel, or pharmacist. Associate members may not vote or hold office on a National level but reap all the other benefits of membership.
The Board will explore a formal mentoring process.
The membership dues will be increased by $15/year starting in July 2002 (That’s $1.25/month extra! That’s not much!). Dues will be $80. Members can opt for three consecutive credit card payments if they don’t want to pay $80 in one sum.
Portable Periop Workshop for RNs - to recruit RNs into the OR. It’ll be a three day workshop. AORN is taking the show on the road! AORN will work on this program and there will be a report at the 2002 Congress.
The epidemic of bovine spongiform encephalopathy (BSE) in the United Kingdom, which began in 1986 and has affected nearly 200,000 cattle, is waning to a conclusion, but leaves in its wake an outbreak of human Creutzfeldt-Jakob disease, most probably resulting from the consumption of beef products contaminated by central nervous system tissue. Although averaging only 10-15 cases a year since its first appearance in 1994, its future magnitude and geographic distribution (in countries that have imported infected British cattle or cattle products, or have endogenous BSE) cannot yet be predicted. The possibility that large numbers of apparently healthy persons might be incubating the disease raises concerns about iatrogenic transmissions through instrumentation (surgery and medical diagnostic procedures) and blood and organ donations. Government agencies in many countries continue to implement new measures to minimize this risk.
From www.cdc.gov/ncidod/eid/vol7no1/brown.htm
A prion is a protein with no nucleic acid and is resistant to standard methods of inactivation. It is acquired from eating cattle and is NOT airborne. Dr. Martin Favero (Director of Scientific and Clinical Affairs of Johnson & Johnson) said it was the “bovine soylent green.” I knew we science fiction fans were in the minority because hardly anyone laughed (I certainly laughed!). There was a 1973 movie called Soylent Green. It was 2022 and the starving masses depend upon the government manufactured food item Soylent Green to exist. But in the midst of a murder investigation, a cop (Charelton Heston) uncovered the chilling source of the product...Soylent Green was PEOPLE! I digress but that was such a great analogy!
Prions are not transmissible from the environment. They are transmissible only through tissue contact. There must be thorough cleaning, disinfection, and sterilization. Someone asked about tonometer cleaning in ophthalmology offices - was it acceptable to wipe the end with an alcohol swab. Because the tonometer (which measures intraocular pressure and is placed directly on the cornea) touches a mucous membrane, it should be sterilized after each use. All instruments that come in contact with mucous membranes and can be sterilized should be
There are four categories of risk associated with Creutzfeldt-Jakob disease (CJD):
High - brain, dura mater, spinal cord, cornea
Medium - lymph node, tonsil, pituitary gland, cerebrospinal fluid
Low - bone marrow, liver, lung, thymus, blood
None - feces, skin, saliva
There is incomplete inactivation of prions with all the usual chemicals and sterilization methods we normally use. With devices contaminated by high risk tissues such as brain and spinal cord, they should be discarded if they are difficult or impossible to clean (remember the prions are not transmissible on environmental surfaces so disposal is acceptable but if there’s visible residue of tissue on a surface, wipe it with a 1:10 dilution of chlorine bleach). Or they can be decontaminated initially by sterilizing at 132-134C for 18 minutes in a prevacuum sterilizer or 121C for one hour in a gravity displacement sterilizer or soaked for one hour in 1 N NaOH for one hour before terminal cleaning, wrapping, and sterilization by conventional means.
For devices that can be cleaned (with disposable brushes!), and there’s effective and total tissue removal, they can be sterilized at 132-134C for 18 minutes in a prevacuum sterilizer or at 121C for one hour in a gravity displacement sterilizer. There was a lot of emphasis on the use of disposable brushes for the flexible scopes and any lumened instrument. Tissue remains on the brushes - and if it’s brain tissue infected with prions - you spread that brain tissue to the next scope you clean with that brush. There was much concern about flexible GI scopes but feces is listed in the “no risk” category. We were encouraged to all use disposable fraiser suction tips in neurosurgery because the lumens are difficult to clean and brain and spinal cord are in the “high risk” category.
The Centers for Disease Control and Prevention’s (CDC) web site at www.cdc.gov has a tool bar on the left side that has the “Emerging Infectious Diseases Journal” listed. Click on that and then type CJD into their search window and you’ll find much information.
Dr. Favero said the CDC was coming out with new CJD guidelines in April 2001.
There have only been two confirmed and four unconfirmed cases of CJD transmitted by surgical instruments. They were 1953-1976 in Europe. The two confirmed cases were due to poor cleaning and inadequate or no sterilization. That news improved my outlook on CJD!
Congress was wonderful as always. The Alameda County delegation stayed at the Ramada Plaza Hotel - a mere ten minute walk to the convention center. On those cold and windy days, I took the free shuttle van provided by the hotel (as did many others!). Congress week started off with a bang - literally. There was a spectacular thunder and lightening storm on Sunday night that started on the stroke of midnight. I have never seen a storm like that - certainly not in California but not in central New York State (where I lived for 23 years) either. I stood at the window mesmerized and watched the sky as it became completely illuminated and then the thunder resounded loudly. The rain came down in sheets and gusted along the streets. The lights in the distance dimmed for about 30 seconds and I wondered if there was a power outage but the hotel parking lot lights were blazing. I guess the rain just came down so much harder that it obscured the lights. I’ve never seen it rain that hard!
The next day, I scoffed at a friend (who’s a native of Illinois) when she said she had to reprimand her roommate to move away from their window and to close the drapes due to her fear of the window blowing in from tornado-like winds. Imagine my surprise when I read in the “Dallas Morning News” that there was a celebration in Fort Worth and Dallas to commemorate the March 28, 2000 tornado that destroyed much of the Fort Worth downtown and blew out windows in downtown Dallas! I’m glad I didn’t know we were in tornado country!
It had been humid Saturday and Sunday but after that storm Sunday night, Monday was a gorgeous, sunny, dry day. I was astounded. People in Dallas continually repeat, “If you don’t like the weather now, just wait a minute and it’ll change.” They’re right!
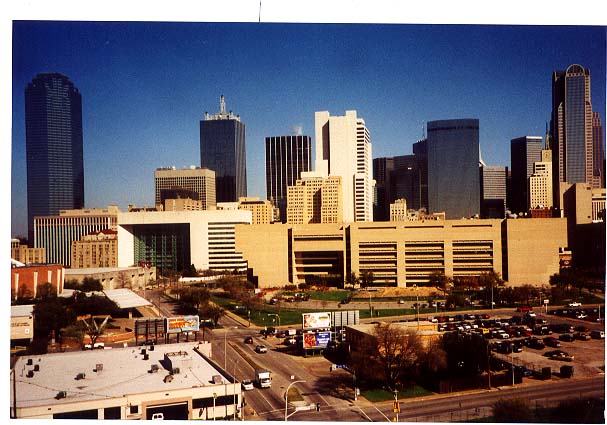
The weather was great the rest of the week except for Wednesday when the Foundation sponsored a free luncheon at the top of the Hyatt Hotel Reunion Tower with fabulous views of the city and the wonderful downtown buildings (I just loved the different architecture found in Dallas!). I went on the outside observation deck and it was unbelievably cold and windy! The atmosphere was much more amenable in the highest area in the tower - the cocktail lounge (which rotated but wasn’t serving any drinks at that hour). I had a perfect view of the Texas School Book Depository and the grassy knoll and all the beautiful Dallas buildings. The rain stopped during lunch and the sun was out so the views were great. The Foundation sponsored an excellent speaker to present information about estate planning. I came away with a lot of valuable information.
The AORN Foundation has started a “Legacy of Leadership.” If you make or modify your will to include the Foundation within the next year, you can become a charter member of the Legacy of Leadership. I have information so you can contact me (marymac@hotpop.com) or contact the Foundation. Obviously, proof of the Foundation being remembered in your will is needed (specific dollar amounts aren’t necessary to include in the documentation to the Foundation). There are many ways to leave the Foundation money while also leaving your family members secure. The Foundation will provide you with this information.
I was disappointed to see the room was set up for about 70 people. Every place setting at the tables for ten had salads and iced tea. I counted about 20 people in attendance! So the Foundation had to pay for 50 uneaten lunches! What a sad waste of money.
2001 Slate
Winners have the highest number(s)
PRESIDENT ELECT (One to be elected)
Donna S. Watson - (Washington) - 794
Vivian C. Watson - (Mississippi) - 450
TREASURER (One to be elected)
William J. Duffy - (Illinois) - 932
Clarence (Butch) A. Fenton - (Maine) - 314
BOARD OF DIRECTORS (Four to be elected)
Katherine Donahoe - (Pennsylvania) - 207
Debra L. Fawcett - (Indiana) - 733
Paula R. Graling - (Virginia) - 946
Jeanne K. La Fountain - (Ohio) - 370
Sheila Ann O’Connor - (Colorado) - 494
Joanne (Jody) V. Porter - (Pennsylvania) - 478
Anita Jo Shoup - (Washington) - 838
Deborah G. Spratt - (New York) - 286
Debora S. Tanner - (Virginia) - 563
NOMINATING COMMITTEE (Two to be elected)
Becky A. Birchfield - (Alaska) - 305
Sylvia Durrance - (California) - 584
(From San Francisco/Marin chapter! Hooray Sylvia!)
Jane H Flowers - (Maryland) - 449
Antonia B. Hughes - (Maryland) - 532
Rudy J. Mancuso, Jr - (West Virginia) - 363
Shirley A. Norris - (Mississippi) - 212
The 2001-2002 AORN Board of Directors follows. Newly elected officers and Board members are indicated by an asterisk (*).
President—Sheila L. Allen, RN, BSN, CNOR, CRNFA
President-Elect—Donna S. Watson, RN, MSN, CNOR, ARNP, FNP-C
Vice President—Betty J. Shultz, RN, CNOR
Treasurer—William J. Duffy, RN, BSN, MJ, CNOR
Secretary—Mary Jo Steiert, RN, CNOR
Board Members:
Michelle Burke, RN, MSA, CNOR
Lorraine J. Butler, RN, BSN, MSA, CNOR
Debra L. Fawcett, RN, BSN, MS
Paula R. Graling, RN, MSN, CNOR
Sharon A. McNamara, RN, MS, CNOR
Anita Jo Shoup, RN, MSN, CNOR
Debora S. Tanner, RN, BSN, MSM, CNOR
Board members may be contacted by writing to them at AORN Headquarters, 2170 S. Parker Rd., Suite 300, Denver, CO 80231. Correspondence is forwarded to them weekly. You may also leave a voice message for Board members by calling (800) 755-2676, ext 311.
2001-2002 Nominating Committee:
Kathleen A. O’Toole, RN, BS, BSN, CNOR
Linda L. Savage, RN, BS, CNOR
Pat Hickey, RN, BSN, MS, CNOR
Sylvia Durrance, RN, BSN, CNOR
Antonia (Toni) B. Hughes, RN, MN, CNOR
Advisor—Brenda C. Ulmer, RN, MN, CNOR
Information from www.aorn.org/congress/election.htm and from posted election results outside the AORN office in the Dallas convention center