(S. A. Patney: Strabismology Desk Reference, chapter
48, JKA Publications)
PARALYTIC STRABISMUS: DOUBLE DEPRESSOR PALSY
One of the rarest conditions in ocular motility disorders, double depressor palsy is
also known by the name of "Monocular depression Deficiency (MDD)". Double
depressor palsy (DDP) is an intriguing condition. This is because its etiology is still
not clear.
In this condition there is a unilateral or
monocular paralysis of downgaze, which means that there is an absence or gross
limitation of the affected eye in dextrodepression, direct depression and levodepression.
That is to say that all the ductions of the affected eye in downgaze are absent or
severely restricted.
Incidence
Double depressor palsy is a very rare condition. The
reports in the ophthalmic literature suggest that usually it is congenital and sporadic1,
2 and 16. I have seen only one case in more than four decades and that was a
congenital DDP. However, literature in neurology has quite a few reports of DDP, several
of them acquired3, 4, 5, 6, 7, 8, 9 and 10. The reason for the rare occurrence
of this disorder lies in the fact that one of the depressors (inferior rectus) is supplied
by the inferior branch of the 3rd cranial nerve and the other depressor
(superior oblique) by the 4th cranial nerve (CN).
Some of the cases appearing to be those of double
depressor palsy are in reality cases of partial 3rd CN palsy. The depression by
superior oblique (SO in adduction) can not be demonstrated because the eye can not be
adducted, the medial rectus being affected too). In these cases presence of intorsion on
attempted depression will show that SO function is intact.
(*A blowout fracture of the orbit may cause inferior
rectus palsy by direct injury to the muscle or by entrapment of the inferior rectus at the
fracture site. ** Scarring in the superior rectus is either due to injury or surgery)
Etiology
The double depressor palsy is usually the result of
one of the following:
- A primary paralysis of inferior rectus muscle, congenital
or acquired
- A primary supranuclear palsy of depression (downgaze)
- A secondary dysfunction of the inferior rectus due to
ipsilateral superior rectus contracture
As indicated earlier, the etiology of DD palsy is
baffling to say the least. The following anatomical facts have to be taken into account
before trying to find the cause of DDP in a patient.
- The two depressor-muscles involved are supplied by
two separate cranial nerves, i.e., the inferior rectus by the inferior branch of the 3rd
CN and the superior oblique by the 4th CN.
- Unlike elevation (upgaze) in which the supranuclear
fibres decussate through the posterior commissure, the depression (downgaze) fibres do
not.
- Supranuclear fibres of depression (downgaze) are
present bilaterally in the rostral interstitial nucleus (riMLF) in midbrain. That
means that for the double depressor palsy (DDP) or monocular depression deficiency (MDD)
to occur the lesion has to be bilateral, making it a rare disorder.
- The blood supply to riMLF and the tract below between
the midbrain and the oculomotor nuclei comes from the paired posterior thalamic paramedian
arteries11 and 12. Bilateral blockage is required to cause a DDP except when
there is a vascular anomaly12 as detailed below. There are three variations of
paired posterior thalamic paramedian arteries. One, each artery arises from 2
separate basilar communicating arteries. Two, each artery arises from the vascular
arcade formed by the Basilar communicating arteries. Three, both the arteries arise
from a single Basilar communicating artery.
If the third variant of the posterior thalamic paramedian arteries is there, an
occlusion of a single vessel can cause ischemic lesions of riMLF on both sides leading to
downgaze palsy. For a more detailed account see reference no. 4.
- Other sites reported as being affected by lesions
having caused DDP are the interstitial nucleus of Cajal, the periaqueductal grey matter6,
7 and 8 and the posterior commissure.
To sum up, the etiology is as follows:
(1) Congenital palsy of inferior rectus alone or accompanied by superior oblique
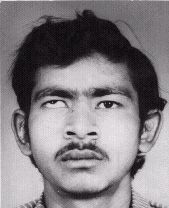
Figure 48-a and b, preoperative and
postoperative (respectively) photographs of a case of cong. DDP (differential diagnosis:
Cong. Aplasia of inferior rectus muscle). Surgery performed: trans-position of both
horizontal recti to insertion-site of inferior rectus. For details see case report 48-1
| Case report 48-1 A 19 years old male patient came with a large right
hypertropia of 35 degrees (77 PD). He had anisometropia with high mixed astigmatism in
right eye. There was moderate amblyopia OD (strabismic, ametropic and anisometropic) with
6/18 (corrected) vision OD and 6/6 OS. There was no binocular vision but the patient could
alternate despite the large deviation. No depression (downgaze) was possible and the eye
remained in horizontal meridian.
Surgery: Transposition of medial and lateral rectus muscles to inferior rectus
insertion was done. The inferior rectus was found to be almost nonexistent. There was a
friable membranous structure in its place attached to the inferior rectus insertion site.
There was no visible muscle tissue.
Postoperative angle of deviation was RHT12 degrees. Second stage surgery (superior
rectus recession) was planned but he did not turn up for it (satisfied with only improved
appearance?). Surgery on SR would have also allowed a look at superior oblique, whether it
was absent or present. He has not come even for a check up for the last many years.
Comments: A total absence of SO function also prompted the diagnosis of DDP but it
could very well be congenital inferior rectus aplasia with or without SO aplasia or
hypoplasia. As the superior oblique has not been exposed, the possibility of SO aplasia or
hypoplasia remains.
|
paralysis. In the latter case the inferior rectus
palsy may be due to a partial III CN paralysis that is associated with IV CN palsy.
Congenital absence of inferior rectus muscle has been reported13. The lone case
of DDP operated in my clinic many years ago (figure 4..-a & b above) also had a
congenital absence of the inferior rectus muscle (case report 4..-1 below).
(2) Acquired DDP
Although congenital DDP has been described as being
more common in ophthalmic literature1 and 2 many more acquired cases of DDP
have been reported in Neurological literature than in ophthalmic journals3, 4, 5, 6,
7, 8, 9, 10, 11 and 14. A case of DDP after hemorrhagic conjunctivitis has also been
reported5.
- Most of the acquired cases, however, are due to
cerebrovascular disease involving the pons and the cerebellum3, 4, 8, 9, 10, 11 and
15. Patients in this group are usually unconscious when they are first examined and
therefore under the care of a neurologist or a physician.
- Trauma to the orbit causing blowout fractures
entrapping or injuring the inferior rectus muscle can also cause monocular downgaze
deficiency (MDD).
- Monocular downgaze deficiency (MDD) may be secondary
to superior rectus contracture after strabismus surgery.
Symptomatology
The main points are as follows:
- Thorough general systemic, neurological and
ophthalmologic examinations should be carried out as a matter of routine and also to rule
out associated cerebrovascular disease in cases of acquired DDP.
- A careful history to rule out previous strabismus
surgery involving SR or IR.
- Congenital cases usually do not complain of diplopia
as they have already developed suppression due to a constant strabismus. However, diplopia
is a common complaint in acquired cases.
- Traumatic cases present with varying symptoms after
orbital injury involving the inferior rectus muscle.
- Doll’s eye movements or vestibulo-ocular
reflexes usually are intact on downgaze (on moving the head from side to side the eyes
move simultaneously to the opposite side). This supports the view that DDP is a
supranuclear disorder and the nuclear reflexes are present.
- Sometimes pupillary anomalies may be there12.
- On orthoptic examination the findings are
fairly typical:
- In primary position there is marked hypertropia.
- Gross limitation of downgaze or depression: The
infraduction of the affected eye is limited in all three directions (direct depression,
dextrodepression and levodepression).
- Upshoot of the affected eye in adduction and
abduction
- Overaction of the affected eye in elevation in all
three directions (dextroelevation, direct elevation and levoelevation).
- Convergence may be found to be defective. This may be
secondary to a longstanding constant hypertropia leading to disuse of convergence.
- Amblyopia, suppression and loss of binocular vision
in long-standing cases
- Upper lid retraction may be present in primary
position with the sound eye fixing. This is because of the attachments between the
superior rectus and the levator palpebrae superioris12.
- Pseudoptosis in downgaze when the affected eye does
not depress but the upper lid goes down (droops or depresses)12.
Differential diagnosis (Table 48-1 and 48-2)
Table 48-1:
| Conditions
simulating congenital MDD or DDP |
Differentiating
features between DDP and this condition |
- Vertical Duane’s syndrome
- Congenital aplasia of inferior rectus (IR) (13)
- Congenital aplasia of IR and superior oblique (SO)
- Congenital fibrosis of superior rectus muscle
- Palsy of 3rd CN-inferior division
|
- Retraction is present in vertical ductions and the
forced duction test is positive (negative in DDP).
- Clinically not possible to distinguish, only surgery
can do it.
- Only surgery can decide
- Positive forced duction test and surgical exposure.
- Exotropia and sometimes pupillary anomalies are +.
|
Investigations
Apart from the tests mentioned above under
symptomatology the following tests should be done if possible:
Table 2:
| Conditions
simulating acquired DDP |
Differentiating
points between DDP and this condition |
- Thyroid ophthalmopathy with superior rectus
contracture
- Consecutive IR palsy due to too liberal a recession
of IR
- Orbital blowout fracture involving IR
- Consecutive IR palsy due to scarring of SR after SR
surgery
|
- Easily distinguished by the presence of thyroid
ophthalmopathy
- Suspected by history of surgery for vertical
strabismus. Only further surgery can decide.
- History of trauma and evidence of orbital fracture
and may be, IR entrapment
- History of surgery for vertical strabismus. Further
surgery can decide.
|
Investigations
Apart from the tests mentioned above under
symptomatology the following tests should be done if possible:
- Forced duction test is a must, particularly to rule
out the presence of fibrosis/scarring/contracture of superior rectus muscle and also of
the inferior oblique.
- If facilities are available CT scan (computed
tomography) of the brain and orbits: The latter is especially useful as it can give a good
idea of the condition of the extraocular muscles, e.g., aplasia, hypoplasia or
fibrosis/contracture.
- Other more specialized tests like recording of
saccadic velocity,
- Electromyograms and
- Magnetic resonance imaging can be of help and are
usually required for research purposes.
Management of monocular depression deficiency or
double depressor palsy
- Nonsurgical treatment
consists of routine
correction of refractive errors and treatment of amblyopia if indicated.
- The treatment of DDP is basically surgical.
- The procedure of choice, in the absence of superior
rectus contracture, is a transposition of the horizontal recti to the IR insertion site.
The horizontal rectus muscles (medial rectus and lateral rectus) are detached from their
insertions and transposed to the inferior rectus insertion.
- If, after the transposition procedure there is
residual hypertropia of the affected eye, recession of superior rectus is carried out in
second stage.
- However, if there is a contracture of superior rectus
muscle as diagnosed by positive forced duction test, superior rectus recession is the
first procedure to be carried out 13 and 17.
- Postoperative complications
are the usual ones
encountered after strabismus surgery, i.e., diplopia, undercorrection, overcorrection and
anterior segment ischemia.
References
- Noorden, G.K. von: Binocular vision and Ocular
Motility: Theory and Management of Strabismus, 5th edition, 1996, St. Louis,
Mosby-Year Book, p. 417.
- Noorden, G.K. von and Hansel, R.: Clinical
characteristics and treatment of isolated inferior rectus paralysis, 98:253, 1991.
- Trojanowsky, J.Q. and Lafontaine, M.H.:
Neuroanatomical correlates of selective downgaze paralysis, J. Neurol. Sci. 52:91, 1981.
- Trojanowsky, J.Q. and Wray, S.H.: Vertical gaze
ophthalmoplegia: Selective paralysis of downgaze, Neurology 30:605, 1980.
- Prakash, P., Menon, V.M., Gupta, A.K. et al: Acquired
double depressor palsy following acute hemorrhagic conjunctivitis, Indian J. Ophthalmol.
36:35, 1988.
- Ozdemir, N. et al: Downgaze palsy due to
periaqueductal lesion diagnosed by Magnetic Resonance imaging, Ophthalmologica 209:225,
1995.
- Jacob, L. et al: Selective paralysis of downward gaze
caused by bilateral lesions of the mesencephalic periaqueductal grey matter, Neurology
35:516, 1985.
- Jacobs, L. et al: Selective paralysis of downward
gaze caused by bilateral lesions of the mesencephalic periaqueductal grey matter and
commissure of the superior colliculi, Neurology 34:95, 1984.
- Jacob, L. et al: The lesions producing paralysis of
downward but not upward gaze, Arch. Neurol. 28:319, 1973.
- Bogousslavsky, J. and Regli, F.: Upgaze palsy and
monocular paresis of downward gaze from ipsilateral thalamo-mesencephalic infarction: A
vertical "one-and-a half" syndrome, J. Neurol. 231:43, 1984.
- Green, J.P. et al: Paralysis of downgaze in two
patients with clinical radiological correlation, Arch. Ophthalmol. 111:219, 1993.
- Rosenbaum, A.L. and Santiago, A.P.: Clinical
Strabismus Management: Principles and Surgical Techniques, 1998, Philadelphia, PA, W.B.
Saunders Company, p. 280.
- Cooper, E.L. and Greenspan, J.A.: Congenital absence
of the inferior rectus muscle, Arch. Ophthalmol. 86:451, 1971.
- Buttner-Ennever, J.A. et al: Ptosis and supranuclear
downgaze paralysis, Neurology 39:385, 1989.
- Halmagyi, G.M. et al: Failure of downward gaze: The
site and nature of the lesion, Arch. Neurol. 35:22, 1978.
- Cogan, D.C.: Paralysis of downgaze, Arch. Ophthalmol.
91:192, 1974.
- Dunlap, E.A.: Vertical displacement of the horizontal
recti. In: Symposium on Strabismus, 1971, St. Louis, C.V. Mosby and Company, p. 307.