by Jennifer Wohlenberg

The
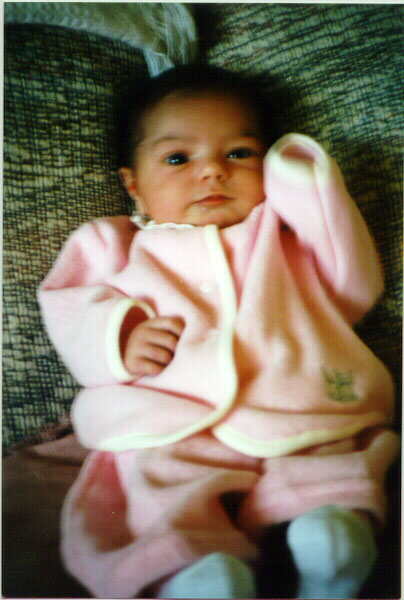
Birth of Ailish Katherine Wohlenberg
by Jennifer Wohlenberg

Anyway, here are the stats:
Ailish Katherine Wohlenberg
7/22/97 12:56 p.m. (scheduled c-section)
9 lbs, 15.8 oz.
22" long
14.5" head
17" shoulders
Apgars 9/9
We got to the hospital at 10:30, and the admitting people showed
us to the exact same room we had last time! He even carried our
bags, so I felt much like we were checking into a hotel rather
than a hospital :) A nurse came in and hooked me up to the
monitors, to check heart rate and contractions. She said,
"Wow, you're having strong contractions 4 minutes
apart." Yeah, I know! Then, she tries to start my IV, and I
have really bad veins, so that was probably one of the worst
parts of the whole experience! She shaved me, and then the
L&D nurse who would be with me through the whole surgery and
recovery came to get me. She's had me before, when I was in for
preterm labor at 26 weeks, so it was like having an old friend.
Both of the nurses commented that I acted like I'd already had 1
or 2 c-sections, because I didn't seem nervous at all. I was just
happy to be getting it over with! She pushed me down to the OR in
a wheelchair, and it wasn't until we got to the room that I
started to get a little nervous. Then the anesthesiologist came
out and explained what they were going to do. I ended up getting
a spinal, which surprised me, because I thought my OB only used
epidurals, but it was wonderful! So much easier going in, and I
didn't end up with a headache, so I was happy with that. They
laid me on the table, and then I heard my dr. talking to Brad and
they came in. My OB said, "Okay, gang, we're doing a
CBAV...cesearean birth after vaginal!" When one of the
nurses asked why, my OB said, "Hey, you weren't here for the
8 days of agony she had to go through the last time
around!" Before I knew it, they were doing the operation. I
started to get pretty dizzy, I guess my BP dropped really low,
and it took quite awhile to get it stabilized.
I was pretty fuzzy there for awhile. I could hear my OB say,
"Suction...no, more suction, more suction!" Then he
said, "Wow! You had an ocean in here!" The assisting OB
then started to push up high, and I honestly thought she was
going to break my ribs. My OB had to use forceps to get Ailie
out, because he couldn't fit his hand and her body through the
incision. She came out absolutely wailing her head off, and I
started to cry. She was sooo big! Everybody there went,
"WOW!" They all took bets on what her weight would be,
and once they weighed her, my OB said, "Weigh her again,
dammit! That baby is 10 lbs!" :) They did the measurements
and everyone in the room said there was no way she would have
come out with shoulders that size, not to mention everything
else, so I felt so good for having gone this route.
Brad brought Ailie over to see me, but then the weirdest thing
happened. I started to feel pain in my uterine area and they
weren't done sewing me up yet. I wasn't sure how much I was
supposed to be feeling, so I tried to deal for a little bit, but
then I started crying, and I asked the anesthesiologist if it was
supposed to hurt this much. He said, "WHAT? You can feel
something?!" So, he quickly gave me a bunch of drugs, which
took the edge off, but I still felt a great deal of the
stitching, and they couldn't even clean me up once they'd closed
because I cried out every time they got near my belly. Everyone
said that was so rare, but I just have a really really sensitive
mid-section, I guess. I told the
nurse about my being able to feel both girls really early in the
pregnancy, plus all the contractions, and she said it was all
probably very related. Anyway, it was over so quickly, and they
moved me to recovery where I, now completely looped on pain
killers, half dozed. I got to my room around 3, still having not
really seen Ailie because of all
that happened after she arrived. They wanted her for extra
observation because of her size, so Brad brought me the video of
the birth and I watched that on the playback of our camera. Once
again, I am *so* happy we got video of it! It was just on the
tripod behind me, and it was enough for me to capture all of it.
I finally got Ailie back at 6:30 p.m., and she immediately began
nursing like a champ. No latch-on problems, she'll do it in any
position, she's wonderful! A tiny bit of tenderness on my
nipples, but nothing like last time, and I think it's just a bit
to get used to.
I started walking once they took the catheter and IV out, and my
OB removed the stitches the next day. He said it was the fastest
healing of an incision he's ever seen! Once the stitches were
out, I felt great! I honestly can't believe how much easier this
delivery was -- everything about it has been much more positive.
Jennifer
Brenna 1/96 and Ailie 7/22/97
Return to Birth Stories
Return
to OPSS Main Page
The Birth
of Zoe Jaqueline Rollo
by Vickie Rollo

I must say that birth is *THE* most amazing thing I've
ever done. I'm staring now at a perfect 7lb,3oz 20" baby
girl named Zoe Jaqueline Rollo and often can't believe she's
ours. Here's our story:
It all started about 3pm Tuesday the 27th. The first contractions
which were quite different than the BH contractions I'd been
getting for a few weeks. These contractions went sporatically
through the evening and into the night. At 3am Wednesday morning
they were about 10 minutes apart, quite reliable and I could no
longer sleep and had to concentrate to get through them. We timed
them until 6am when they were 2-3 minutes apart. We called the
hospital and they told us to wait another 30 minutes and if they
were still that cloe to come in. They immediately went back to
about 10 minutes apart. At 8am they went back to about 2-4
minutes apart so we called again and they told us to come in if
we really wanted to. I did, and was not thrilled with the
response and support (or lack of)
they were giving me. We got in and they examined me. 1cm
dialated. I was crushed! They told me to go home, as it would
still be quite a while (they suggested a day or two!) I couldn't
stop crying. I couldn't tolerate the pain I was in for two more
days!!!! We went home and I managed to get 2 whole hours of sleep
before I was bombarded with contractions. Very painful and barely
a minute between them. I felt I had to pee and poo all the time.
I was also vomiting quite violently. This lasted from 12pm till
3.30pm when I could stand no more. My husband called the hospital
and told them that I was in too much pain. I *HAD* to come in so
they could give me *something*. They reluctantly agreed. I came
in, crying and sobbing. They examined me...6cm! Thank god. They
gave me Nitrous Oxide (sp) Happy gas! It was great. They were
filling up the spa bath for me to relax in and they left to fill
in my computer details and get me all checked in, call the OBGYN
etc. She came back what seemed like 15 minutes later (my husband
says it was almost an hour) and I asked to go into the bath. They
had to examine me again first to make sure I hadn't broken my
waters. She looked up and said "You aren't going anywhere,
you're dialted to over 9cm!" I was thrilled. I started to
push and got yelled at. I wanted to push. I had to pant for a
while. I started pushing, which I think was the hardest part. I
hate to say it, but it felt like taking a really really big poo!
After much pushing and many screams and a little abuse of the
nursing staff, Zoe was born. I didn't have time for an epidural,
so I felt much pain. But I am very proud of what I did. I had 3
stitches from a tear. one up top, two down the bottom. They
caused me very little pain and now, five days later, I hardly
know they are there. I still can't believe we did it. She's the
most amazing thing ever. That's it from me.
Good luck to all you up and comings!
Vickie
Proud Mum of Zoe Jacqueline Rollo born May 28th, 1997!
Return to Birth Stories
Return
to OPSS Main Page
The
Birth Story of Emilee Joanne Nazareth
by Staci Nazareth

It was September in Idaho and 90 degrees, a record heat
wave. I was 13 days overdue with my baby and absolutely desperate
to go into labor. I had tried walking, squatting, eating spicy
foods, but baby refused to be born. Finally, on Wednesday,
September 17th my Dr. admitted me to the
hospital for a serving of prostiglandin gel. My husband and I
watched television, ate and relaxed, hoping that sometime in the
middle of the night I would have contractions and we would
shortly be proud parents.
Boy were we wrong! The nurses had advised me that they would be
waking me at 5:00 a.m. to get me showered and ready for the
Pitocin drip. I was so nervous that I was up at 3:00, doing
crossword puzzles and trying to read magazines. I conked out
again and was upset to wake up at 6:00 a.m. Where was the nurse?
I buzzed and the nurse ran in to explain
that another woman had just come- in full labor. I could hear her
screaming, and my heart started beating faster. While I continued
to wait, another woman came in- also in full labor! These two had
their babies within 15 minutes of entering the hospital- this
gave me a little hope.
Finally, at 8:00 the Dr. came in and asked why I wasn't on
pitocin. He broke my waters at 8:30- which didn't hurt, like I
thought. He had the nurse get me started on pitocin, and at 9:00
I began having mild contractions. Mike held my hand and we moved
about the room as best we
could, what with me having an IV, and 2 monitors strapped to my
belly.
The nurses continued doubling the dose every 20 minutes and the
contractions began to get stronger- but nothing I couldn't
handle. I practiced my Lamaze breathing and squeezed my husband's
hand while watching the contractions peak on the monitor. This
went on throughout the afternoon, until 5:00 when they were
really strong. Contractions were coming every 30 seconds and
lasting about a minute and a half. I was banging my head against
the pillow and groaning when the nurse gave me a shot in my IV
for pain. Finally, relief! I was practically knocked out and
managed to rest for an hour when it really started hurting again.
At 6:00, the Dr. examined me and said I hadn't dilated beyond a 2
or 3. This was so defeating after all that pain. He told the
nurses they were hyperstimulating me on the Pitocin and
immediately stopped the drip. I tried to relax, although I was
crying to my husband. After they slowly
started the drip again, and I got to the point of pain around
8:00, the nurse told me that I should consider having the
intrathecal. The anesthesiologist came around 8:30 and
administered the drugs-
leaving out one important fact- that anesthetic could make you
vomit! I had no idea! Instantly my legs went numb, and shortly
after that Ibegan barfing! I have to thank Mike for cleaning me
up each and every time, as I was sick a lot. I still had pain on
the drugs, and at 10:00,
after examing me and finding I was still only dilated to a 4, the
Dr. told me he had to consider a c-section. I was desperately ill
by this time and anxious to have the pain go away,
so I instantly agreed. At 10:30, they wheeled me to the operating
room and I again was dosed with drugs for the c-section. I was
sweating profusely, but they had my arms strapped down so I
couldn't wipe my face. That made me really upset, as all I wanted
to do was scratch my
nose! I was starting to go in and out of it by this time, but I
do remember seeing my husband come into the operating room in
scrubs and thinking how cute he looked. He held my hand and
looked at me, and again cleaned me up after I continued barfing.
At 11:15 p.m. the Dr. came around the curtain with a bawling,
purple baby. She was screeching at the top of her lungs, and I
was so relieved that she was born! Mike stayed with Emilee for
the 2 hours after her birth and gave her her first bath. They
brought her to me around 1:30
a.m. and she immediately began breastfeeding. The following hour
or two is quite blurry, but I couldn't believe how beautiful she
was.
My beautiful baby is now 2 weeks old and my breath catches every
time I look at her. She is a gorgeous baby with big dark eyes and
a full head of hair. We are so blessed to have her.
 |
Emilee Nazareth
Return to Birth
Stories
Return
to OPSS Main Page
The Birth Story of Susan Michele Mesler-Evans
by Stephanie Mesler-Evans

On Sunday, the 5th, around 12 midnight, I
began to have contractions. We called both midwife and substitute
OB (the evil Dr. Reich), and were told to go ahead to Labor and
Delivery at Grant Medical Center. When we got there, we learned
that I was only 2 cm. dilated and that the contractions were not
regular and we were sent home because this
was not "real labor."
We got home around 5 a.m. and went to bed. Around 7:30 a.m., I
woke up feeling that I had to pee. When I stood up, fluid
*gushed* out of my vagina. "Gee," I thought,
"maybe my water broke." But we had had so many false
alarms that I didn't want to rush to the hospital just to be sent
back home. So I went back to bed. An hour later, I woke again to
the same sense of having to urinate, stood up, and once again
gushed liquid. THIS time I called the doctor, who told me to come
back to the hospital. The strangest part of all this was that my
contractions stopped completely when my water broke. We arrived
at the hospital a little past 11 a.m., and they examined me to
determine that my water had *indeed* broken and told us they
would induce labor if contractions didn't start soon.
Around 3 p.m., induction by Pitocin was begun. I immediately
began contracting and proceeded to labor until about 3 a.m.
During the labor, I received Nubain (sp?) and an epidural for
pain, which was excruciating nonetheless. By 12 midnight on the
sixth, I had begun to sense something was wrong--I was laboring
hard and my cervix still was not
opening all the way. I was in enormous pain and started to wonder
if a C-section would be necessary.
Around 3 a.m. on 10/6, I began to push. My cervix had dilated to
10 cm. and I was in agony. I *pushed* for about three hours at
that time when the doctor arrived. At that point, I told him that
something was wrong and that I wondered if we shouldn't be
talking about a C-section. At that point, I had been in labor for
30 hours, pushing for 3. The evil
Dr. Reich (TEDR) refused to let me stop pushing, and proceeded to
examine my cervix during a contraction without warning, and
refused to remove his hand when I started screaming. I ordered
him to take his hand out of my body until I could get through the
contraction, and he refused. He was trying to feel for the baby's
head, which I knew he couldn't reach, because I could tell she
was stuck further up in the birth canal.
Between 6:30 and 7, I announced that I had to have a break,
demanded that the Pitocin be shut off, and that I be given some
more painkiller, which had been shut off since around 3 a.m.--I
was just too tired and in too much pain to continue. TEDR told me
I hadn't been working hard enough, and that he would give me this
break *only* if I
promised to "work harder after." So I rested through
contractions until about 10 a.m., when TEDR returned to the
birthing suite to direct my labor. The Pitocin was turned on
high, epidural turned off, and I pushed approximately two more
hours on the birthing ball.
As a last-ditch attempt at a vaginal delivery, TEDR tried
todeliver Susie by vacuum suction (!). It hurt like hell and did
not work. I bled *a lot*. Finally, around 12 noon on the 6th, it
was decided that I would have a C-section after all. Susie was
born at 1:13 p.m. (EDST) and has been goin' strong ever since!
What bothered me most about my birth experience was not being
listened to. I kept telling the doctor, nurses, and midwife that
something was wrong. We already knew that I was having a large
baby, and that God had cursed me with an android-style pelvis
(meaning narrower at the bottom than at the top). I kept telling
them I thought she was stuck, and nobody listened. I labored for
36 hours, pushed for six, ended up
bloody, beaten, and emotionally torn up for no reason at all. In
the end, I have to say that I think C-sections are way cool ;-) I
had a spinal for pain, and was wide awake when Susie was born,
although I didn't even know the surgery had begun until I heard
her cry.
Until then, I managed my terror and stress by singing kiddie
songs at the top of my lungs. I did everything from "The
Baby Bumblebee Song" to "Tomorrow" (from ANNIE).
Part of the time, the hospital staff sang along :-). Weird, I
know, but it got me through the scariest experience of my life
(to that point).
Paul was there through the whole thing--he took Susie from the
doctors as soon as she was born, helped get her cleaned up, and
brought her to me while they sewed up my incision. He was a great
support. After delivery, I was taken to recovery, where I held
Susie for the first time. She has hardly left my side since then.
I stayed at Grant Medical Center until Friday afternoon, 10/10,
when my staples were removed and we were released. Throughout the
week (and the weeks before), I had been experiencing shortness of
breath. TEDR kept telling me it would go away on its own.
We arrived at home around 7 on Friday night. By 11 p.m., I had
been taken by ambulance to Riverside Methodist Hospital, where I
was treated and admitted for congestive heart failure. It was
also discovered that my blood count was dangerously low and I was
treated for that. On Monday morning, I had another ultrasound on
my heart, which
showed there _is_ damage to my heart. However, my heart is
functioning fine and after treatment for the congestive heart
failure, I am feeling great! (Well, as great as anyone could feel
under the circumstances. At least I'm breathing!) Monday morning,
as I was giving myself a sponge bath in the hospital bathroom, my
C-section incision gaped open. Thank God I was in the hospital
when it happened! I called for the nurse, who called for a
doctor, who called for an OB (not TEDR), who re-stapled my
incision. I learned at that time that the staples should not have
been removed for 10 days after delivery (at least!). Mine were
taken out after four. Monday afternoon, we came home again. This
time, I hope we get to stay!
As a result of all this, I am unable to breast-feed. This is
partly due to the radiation during the tests on my heart and
lungs, and partly due to the fact that I am now taking Prozac. At
Riverside, I spoke with a social worker and psychiatrist, and we
all agreed that my birth experience, combined with the trauma of
the heart failure, and post-partum
depression, required treatment with drugs and therapy. I had a
hard time with this at first, but decided my baby is better off
with a stable, healthy mama than breast milk. Someday she'll
thank me!
Return to Birth
Stories
Return
to OPSS Main Page
The
Birth Story of Bridget
Kerrianne
by Chris McGuigan

When I went for my doctor's appointment
on Friday, October 3, I was
already planning to beg him to induce my labor. I was 3 days
overdue,
and this kid was just not getting any bigger! The doctor agreed
to
induce the following Monday if "nothing happened"
before then. Then he
saw that my blood pressure was a little high, and my urine was
showing
1+ protein. He sent me downstairs for a non-stress test and
ultrasound. They both turned out ok, and my bp had dropped
slightly
when I went back to talk to him again, but a second urinalysis
showed 1+
protein again. So he had the nurse catheterize me for a better
sample.
Ow! Anyway, no change, so he decided to send me to L&D to be
observed.
If I did have toxemia (which I had in my first pregnancy), I
would be
induced in the morning. If not, I would come back to be observed
again.
Well, we went to L&D, with a quick stop at my mom's to let
her and
Mikey know where we were going. We got there around 6:30 Friday
evening. They immediately put me on the fetal monitor, with an
automatic blood pressure cuff checking my bp every 15 minutes
(and yes,
I insisted on the large cuff, which I had also done at each
doctor's
visit). It was still slightly high, and my urine was still
showing
protein, so it was decided to admit me to be induced Saturday
morning.
At 10:00 am Saturday, the only doctor in the practice that I
hadn't
met yet came in and introduced herself, saying, "I'll be
delivering your
babytoday." Somehow I knew I'd end up with the one doctor I
didn't know
<G> but fortunately, I really liked her. I was given
pitocin at 10:20.
Shortly afterwards, I started getting cramps that didn't register
on the
monitor, so I assumed they were gas. Wrong! <G> They got
progressively
stronger and closer together. At 11:20, the doctor broke my water
just
enough to use the internal fetal monitor. That's when the
contractions
REALLY got going! By noon, I couldn't breathe through the
contractions
anymore, and was begging for an epidural. The anesthesiologist
was in
surgery, so they called someone else from home. By the time he
got
there and was ready to give me the epidural, I was 5 cm (I was 3
cm when
I was admitted).
I had several contractions while leaning over the edge of the bed
waiting for the epidural to go in, but the nurse was really
great,
helping me breathe through them. DH was useless at that point,
and I
kept telling him to stop showing me how to breathe and get his
hands off
me. Finally, the epi kicked in. I calmed right down (no more
pain!<G>)
and told dh he could watch tv now if he wanted, because I planned
on
taking a nap. :) I dozed off between contractions, until they got
uncomfortable again, around 2:00 or so. The doctor came back in
to
check me, and I was up to 8 cm. By 2:55, I was at 10 cm, and more
than
ready to push. At 3:16 pm, Bridget finally popped out, all 9 lbs.
3 oz.
and 22" of her.
She did give us a little scare. Apparently, her heart rate
dropped
drastically right before she came out, and she passed some
meconium.
They don't think she swallowed any, though, and seems fine. She
also
had low blood sugar, and I had to feed her right away. She
wouldn't
latch on, and it was important she be fed immediately, so they
took her
to the nursery and fed her some formula. Her blood sugar came
back up
then, and there have been no problems with nipple confusion.
Anyway, that's my birth story. I didn't plan for it to be quite
so
long, but I guess I remembered more details than I
thought.<G>
Return to Birth
Stories
Return
to OPSS Main Page
The Birth Story of Meredith Meaton
by Paula Meaton

Here is my birth story for those of you interested. I
woke up Thursday
morning at 4:30am wondering what my 24 hour urine results were. I
managed to wait until 5:30am before calling the lab and getting
the
results. My protein went from 535 to 813 in a week, not good. I
managed
to lay down and sleep some before the Dr.s office opened at
9:00am. I
called and was told the nurse would have to call and get the
results and
check with the dr. At this point I already knew the plan even
though I
was told nothing. I began to pack my bag and waited for the
official
word. I was to go to the hospital and have my NST and biophysical
profile, then have the results called over to the office and wait
to hear
from the dr before leaving the hospital. I was also told to take
my bag
along. I had my NST and passed even though the nurse didn't like
the
look's of the strip. I went for my biophysical profile and only
got a 4
out of 8 , the baby didn't move which meant 0 for movement and a
0 for
tone. My blood pressure was 182/104. I was told to stay at the
hospital
and to go to labor and delivery.
Once in labor and delivery I was put on an IV with pitocen,
magnesium
sulfate, and glucose. I had the head of anesthesiology come in
and said
she was going to take a look at my back, then wash it with
betadine, and
numb a spot with novocaine. I said WHAT!!!!!!!!!!! She kindly
explained
she was going to give me an epidural, I said NO WAY!!!!!!!!!!!!!!
She
again explained that it was necessary because I was at high risk
for a
c-section, I still said no, then the nurse got in on it, and I
still said
no, then they got the Dr in on it, I still said not, we debated
for
several minuets. I guess what really ticked me off about the
whole thing
was I was never consulted, about it. I eventually agreed, was
made them
aware of the fact I was not happy about it. The anesthesiologist,
poked
me 7-8 times and failed (or so she said) every time, she said
that the
needle was not long enough and they didn't make them any longer
and that
I was a hard stick because of all of my extra layers. She really
ticked
me off. After her 3rd attempt I asked for some one else, but she
kept
trying. I was given a hour off, and was started on all of my IV
med's
again. The next person came in and with one poke had the epi in
place
and working. She went through more layers then the 1st person,
and with
better success. I then had a catheter put in place because I was
not
allowed out of bed due to the Mag sulfate. By now it was 7pm and
the
pitocen was doing nothing, I was hooked up to a blood pressure
cuff which
went off every 15 min's, and I had continuous fetal monitoring.
Talk
about all the wires.
Through the night nothing happened, 6:30 am they decided to
rupture my
membranes, WOAH NELLY!!!! I began having contractions
immediately, my DH
and Mother who had been with me all night decided to go to
breakfast
about 7:30am, when they came back I was begging for the drugs to
be put
in the epidural, this was about 8:30 or so. The doctor came in
and
checked on me at 9:30 and I had dialated form a 2-3 at admitting
to a
4-5, not a lot of progress, they discussed it and said probably
some
where around 4 pm if I went by normal labor progress. 45 minuets
later I
had to PUSH!!! Mom said no, not yet, I said OH YES YET!!. The
nurse
came in I was dilated to 9 1/2 cm and was having contractions
close and
hard, time to Push. I pushed for about 1 1/2 hours and Meredith
was here
at 12:03pm. Her lungs were not doing as well as they would have
liked so
I only had a few minuets with her before she was taken to the
nursery for
close monitoring. The dr began doing his internal exam and
discovered
that the epi didn't do it's job, boy did that hurt. I had a
laceration
internally needed stitches for that, but no episiotomy, so I
guess I was
lucky. I didn't need to have any external stitches. The dr began
waiting for the placenta, and nothing happened. He began talking
about
doing a d/c under general anesthetic, but because the baby was
still in
the room I talked him in to waiting a little longer then the
usual 20
min's and was given 30. The placenta finally came out and it was
time
for the stitching, ouch what a sting those little numbing needles
make.
I was left in labor and delivery for 24 hours due to all of the
medications, oh yes, he added insulin to my IV too about an hour
before
delivery, I am not too sure why, I was pretty out of it. Those
meds
(mag sulfate) are pretty mind blowing. I was moved to OB special
care
unit, and released on Monday. Meredith was not released until
Friday
10/31 due to jaundice and a large weight loss. we are all home
and doing
well.
Meredith was born on 10/24/97, 7lbs 1oz, 20 1/2" . Her
weight dropped to
6,1 and was up to 6,3 when we cam home.
For those of you wondering, I would do it all over again, and was
already
wondering when we should start trying again, after all it took us
2 1/2
years to conceive this last time.
Return to Birth
Stories
Return
to OPSS Main Page
The Birth
of Rowan Justina
Weller
by Heather Weller

Rowan Justina Weller was
born Thursday November 6th at 4:50 pm. She
weighed 6 lb, 13 oz, and was 19.5 inches long. Ever the stubborn
baby, she
managed to keep her gender secret until about 5 minutes after her
birth as
she was whisked across the room by the NICU staff before the
doctor could
see (more on that a little later).
We got home from the hospital Saturday afternoon, and are doing
well -
though Gary still can't stand to hear her cry, and feels like
he's a
personal failure every time she does (which makes getting him to
change
diapers a bit tough).
Anyhow, as briefly as i can - her birth story. We went into the
hospital
Wednesday morning to start the induction. Although i'd told
everyone not
to expect we'd definately have a baby by that evening, i think
that was
still the expectation. I'd agreed to take part in a study of a
different
form of prostaglandon (i will some day learn to spell that) than
the gel,
so for 24 hours, every six hours i had to take a pill and have a
vaginal
suppository inserted. When i went into the hospital, i was 1 cm
dialated
and 20% effaced. 24 hours after the treatment was started, i was
3 cm
dialated and 80% effaced, not very reassuring.
The whole time i was on a magnesium drip, which really is the
strangest
thing. Although i was aware of what was going on all the time,
there's
still a hazy kind of memory about lots of this stuff. It's kind
of like
when you're drunk and then start to sober up a little, and think
you're
really sober, then realize a little later you were still slightly
drunk
(um, college flashback, whee!).
Anyhow, at 12:30pm Thursday they began the Pitocin. For the first
hour i'd
have occasional contractions, which for some reason would NOT
show up on
the contraction monitor (they were real, the nurse could feel the
tightening, i could feel all kinds of stuff, but nothing would
register).
They noticed every time i would get up to use the rest room the
baby's
heart would decelerate, so after about 2 hours, i ended up
entirely
confined to the bed. Out of the blue, the contractions were
coming all
over the place, i was clawing the bed in pain, Gary was sitting
in the
chair next to me crying, and then i suddenly had to vomit. Yay, i
think,
i'm in transition, this'll end soon, i can make it.
They came in to do another internal exam - i was all the way
dialted to....
*four* lousy centimeters. Now, at this point, i'm breathing as
well i can
through each contraction (except the few when i would just sit
there and
chant "i can't i can't"), and i still feel like i'm
going to die if all
that was simply to get 1 more centimeter dialated.
At this point, i'm pretty fuzzy on time and such. I pretty much
ended up
in my own little world wanting to be anywhere but where i was.
Now, if i
had to do this all over again, this is where i'd have made sure i
had
written my birth plan for someone other than my poor husband who
couldn't
stand to watch me in pain enough to do as i'd wished. I'd wanted
to have
to wait about 15 minutes after requesting any medications before
getting
it, to see if i could make it through. I'd also wanted to try a
shot of a
narcotic before going for the epidural if i needed something. But
let me
tell you, the second they asked if i wanted something for the
pain
(reminding me i might have to wait a bit since i was still only 4
cm
along), i jumped at the chance.
So, my obstetrician came in and checked, and all the sudden i was
crying
that i'd wet the bed. I was totally horrified at the thought (i'd
tried
w/o much success to use the bedpan a bit earlier). Well, turns
out the
water had actually broken. It was around 4pm when the doctor
approved
medication, and offered me the choice of an epidural or narcotic.
I went
for the epidural. So, the anestesiologist (there's that funky
spelling
thing again) came in to put the cathetar in, and warned me it
might take 20
minutes or so for everything to get done and for it to take
effect.
Apparently i'm a bit sensitive to the anestsia they used, though,
because
almost the instant they turned it on, i was a new person. I could
actually
look at people when they talked to me and pay attention to my
surroundings.
On the down side, i coudln't feel much (even my arms were a bit
numbed).
Apparently, though, in the time it took me to get the epidural
in, i'd
somehow dialated completely. Which is a good thing, since Rowan's
heart
rate started to decelerate again. They decided to use forceps to
deliver
her, with me there trying my hardest to push while unable to feel
anything
from the neck down. Before i knew what was happening, they were
whipping
this baby out of me and across the room to the NICU people. We
asked if it
were a boy or girl, and my obstetrician kind of hrmmed and said
"it's a
baby..." A few moments later one of the NICU staff announced
it was a girl :)
She's recovered wonderfully well from her initial rough start in
the world.
Her apgars were 4 and 7, but now, i dare say w/ some bias, she's
perfect.
It was very strange to me, i was so out of it with the magnesium
and the
epidural, i couldn't comprehend that i'd actually just given
birth. It was
about an hour before i was able to hold her, and even then, i was
so numb
in the arms and light headed, i had to ask them to take her back
because i
couldn't stay upright. They did help me nurse her lying down, and
she is
one champ of a latch-on expert.
As my obstetrician said to the resident who actually delivered
the baby "so
much for my non-interventionist style." I know she's fine
now, and that
i'm fine now, and those are the things that matter, but still, if
i had it
to do over again...
I think what has surprised me the most after everything is how
sore i am
still. I mean, i didn't expect to do a jig out of the hospital w/
baby on
hip, but i also didn't expect to still feel as if i had sat on a
meat
grinder. Between the stitches (which actually are not all that
bad) and
the hemmhoroids (which are that bad) and the general tiredness of
everything, just getting up and down can nearly reduce me to
tears on
occasion.
The one problem i'm having now is getting Rowan to eat enough -
she sleeps
so deeply and so much, even if i wake her entirely w/ a diaper
change or
something before starting nursing, she still has to be prodded
and cajoled
to suck for 10 minutes at a time. Last night she would have slept
through
the night if i hadn't woken, and that scares me, because waking
at night
isn't something i do very well. Last night she fed at 12:30am
then not
again until 5am when i woke up on my own. I don't know whether i
should be
ecstatic i'm getting some sleep at night or petrified she's going
to starve
to death!
heather (and Gary, Rowan, and 2 *very* perplexed cats)
Return to Birth
Stories
Return
to OPSS Main Page
The Birth of Megan Jean Thayer
by Kelli Thayer

Born 10/23/97, 7 lbs 5.7 oz, and 20 inches long.
6:08 a.m.: Leave home to go to hospital.
The hospital is 50 miles away. We are going to do an
amniocentesis to see if the lungs are mature. If they are (the
test should take about 30 minutes to do plus 1 - 2 hours for the
results), we will probably induce
7:15 a.m. Am in hospital L & D room waiting for the doctor.
7:35 a.m. The doctor does an ultrasound. It appears that there is
little amniotic fluid. What there is is behind the placenta and
we can’t get to it. We now discuss options. Do we wait for
2+ weeks until I am due and hope nothing happens in the meantime?
The doctor says he would not wait that long due to the very low
level of fluid. There could be problems. We decide to go ahead
and induce - the risks of waiting are more than the risks of
going ahead. Tomorrow I will be 38 weeks and am technically to
term plus 6 days.
8:10 a.m. First application of Prostaglandin E2 gel (aka the Gel)
with internal exam. Exam shows cervix hard, 0% effaced, 0%
dilated. Baby very high up - not even able to feel head although
it feels as if his hand is on my tonsils. Apparently the Evening
Primrose Oil didn’t have any effect on me - maybe because I
didn’t take it long enough.
12:30 p.m. Have monitoring for 20+ minutes every hour plus
monitored for solid hour after Gel application. My dh left at
10:00 to take our daughter to her doctor appointment (ear
infection - all gone now and she is fine) and then to drop her
off at her grandmother’s house (after feeding her). This
involves driving back into town - a hundred mile round trip. Exam
shows minor change in cervix - some softening, however, 0%
effaced, 0%
dilated, can’t feel head. Second application of Gel. Mild
cramping due to Gel.
5:30 p.m. Exam shows cervix now soft, 50% effaced, no dilation,
baby still high up. Third application of Gel. My doctor is going
to go home (he lives in the same town I do) and he will drive
back late tonight (be back around 11:00 p.m.) and stay overnight
to take care of me! What a great guy! The doctor said the baby
will be fine, however, chances of a c-section are 50-50. He
encourages me to continue to hope for VBAC - we can do it!
6:20 p.m. My dh is back with me now. I was so bored without him.
The
television remote didn’t work so...Get up to change channel
and walk as much
as possible - when they aren’t monitoring me. No
contractions as far as I
can tell, however, the baby’s heartbeat is strong and
steady. This was the
longest part of the whole process I think (besides the 9 months).
Still have
cramps - not contractions but they are uncomfortable
nevertheless.
11:00 p.m. Monitoring still every hour. Exam shows cervix 75%
effaced,
fingertip dilation and the baby has moved down now - can feel the
head. Will
start up the IV with Pitocin (aka Pit) shortly.
12:30 a.m. Finally got IV going (left wrist/hand) and slow Pit
drip (12d/hr). Will up the Pit in 20 minutes. They want good
contractions, 3 every 10 minutes at least. Gave me a sleeping
pill also.
2:30 a.m. Very groggy but able to go to bathroom. Contractions
register now - up to 60 on the scale. A bit uncomfortable but
bearable. Can’t sleep very well even with the sleeping pill
- guess I am too keyed up.
4:00 a.m. Contractions are much stronger now. They have been
upped the Pit until they were fairly strong and regular. The
register over 100 on the machine at times. Went to bathroom -
they stop the Pit when I go and the contractions stop. I think I
go to the bathroom just to stop the contractions now.
7:00 a.m. Still lots of pain from contractions. Bearable but I am
getting tired. Probably slept/dozed for less than 2 hours
overnight - even with the sleeping pill.
7:30 a.m. The doctor says 1 cm dilated. He will up the Pit and I
can have the epi whenever I want. I elect to do so ASAP since
they are going to crank up the Pit a lot now.
8:15 a.m. The anesthesiologist put in the epi. It took a couple
of tries but it was still done rather quickly/efficiently. The
worst part was his pressing his fingers into my spine to figure
out where to put it. The deadening hurt slightly - mostly just
the burn from the drugs. I was scared but my wonderful husband
stayed in the room and held my hand. Within a half hour there was
no pain at all. It was wonderful. As the doctor left the
room he said I would be having the baby within 6 hours. We
decided to have a little ‘contest’ to see who could
guess when the baby would be born. We excluded The doctor since
we jokingly said he could always win by just telling me I needed
a c-section and having it exactly when he said. Of course he
would never do that, but it garnered a laugh from most people. My
dh went out and bought a prize - a Halloween bucket full of mini
candy bars. Not much but we are on a bit of a tight budget.
Had catheter put in after the epi took effect. Now cannot get up
but I do have movement - not totally numb.
9:00 a.m. My dh went to get food for himself and find cough
medicine. The person in the hospital pharmacy was nice enough to
give him some cough drops. The contractions slowed down, almost
stopped. The nurse upped the Pit way high to get the contractions
going again. After the initial shot directly into the epidural, I
was not hooked up to the drip. After a bit the epi wore off and
the contractions started again.
9:30 a.m. Last meal - a rather bland breakfast but it’s
better than nothing. I won’t be allowed to eat or drink
(except ice chips) until I deliver.
10:30 a.m. The contractions were almost unbearable. I was crying
and just short of screaming. They were every two minutes and
registered way over 100 on the meter. I asked to be hooked up to
the drip and the nurse complied (around 10:55) - then told me it
would take at least a half hour to take effect AND that it would
only help the pain - not take it away like thedirect shot did.
Yikes!
11:00 a.m. Still no relief. The nurse was a bit condescending -
telling me that this was labor and it was going to hurt, etc. I
felt like strangling her. Thankfully she had called the
anesthesiologist and he came and gave me another direct shot into
the epi catheter. He said about 10-15 minutes for relief and he
was right. A bit later, the drip was starting to work and the
edge was taken off. I had talked to my doctor about having the
epi a little
lighter -not being totally deadened - so I could help push. We
had agreed to this.
12:15 p.m. The doctor finally came. Exam showed that I had
finally made it to 4 cm dilated, 100% effaced and station -1. He
said things would proceed fairly quickly after this. Maximum
would be 1 hr. per centimeter (if things were really slowed down)
- but would most likely be much quicker. It was getting difficult
to get a good reading on the external fetal and contraction
monitors. They were unreliable. He broke my water and hooked up
internal ones. Thankfully the epi had taken effect again and it
didn’t hurt.
12:35 p.m. Exam again - now 8-9 cm dilated! Epi is slow -
contractions hurt
but are bearable. The doctor said he was going to go grab some
soup and be right back. He was counting on another girl
delivering soon, and then me.
12:45 p.m. - Surprise! Exam shows fully dilated! He can feel hair
and said I am ready to give birth! He is a bit taken aback since
he was planning on delivering the other lady first. Well -
I’m ready, she’s not, so....
12:46 p.m. - I am in a bit of shock. More than a bit of shock. I
start shaking and the nurse brings me warm blankets to help. I am
also scared - is everything going to be okay? It just seemed so
quick here at the end. Everything - 9 months of waiting,
wondering, pain, sickness, joy, etc. all about to come to a
completion. It was so quick - I was planning on there being a
couple more hours to get used to the fact that I was about to
give birth!
1:00 p.m. Ready - everything is set up. The doctor convinces my
husband to go to the end of the bed and take a look - you can see
the head and hair! I don’t feel the ‘need’ to push
but am told that I am ready. Then the doctor explains that on the
next contraction, he wants me to take a deep cleansing breath,
then another breath and push while my husband counts to 10. I do
as I’m told, however, it seems like my husband is counting
very slowly. Everything gets blurry, the next thing I know, the
doctor is asking me if
I’m okay. Apparently I had passed out for about five
seconds. How embarrassing! Since the doctor didn’t know why
I had passed out, he said he wanted to deliver the baby by
forceps. I started (or continued - I’m not sure) crying -
worried that everything would be all right. He assured me that
everything would be fine! I took a few deep breaths while he got
the forceps in place. Thankfully, nothing hurt although I could
feel him down
there doing something.
1:18 p.m. Time to take another deep cleansing breath, then
another and push. My darling little girl came right out -
screaming her head off! It was that simple in the end. The doctor
tells me she is perfect (although I was worried that she seemed
so blue - however, apparently that is normal - just the feet and
hands. With the vernix covering it made her almost purple - very
interesting). The doctor offered to let my husband cut the cord -
he
declined but with much more grace than I would have thought. I
saw them cut the cord then whisk her off to the side to do a bit
of cleaning, wrapping up, put on hat, check Apgar, etc. She
scored 9/9! Within a few minutes I got to hold her and I
couldn’t stop crying - I was so happy. I asked my doctor if
everyone cried like that - He said usually someone was crying -
if not the mother, then himself or the nurses!
1:25 p.m. They took her away again for a bit while I finish this
business. My husband went with her since he didn’t want/need
to be there for the messy part. I finally want to push when the
afterbirth is ready to come out. Talk about a good feeling - it
was so weird - one push and it all came out. The doctor showed it
to me - I wanted to see. I know it’s weird but I wanted to
know everything there was about this whole process. It took
another 25 minutes to sew up the 3rd degree tear. Apparently this
happened so fast that
there was no time for an episiotomy. Thankfully I was totally
numb by then from the epi shot (talk about strange timing) and it
was rather fun to converse with my doctor and his assistant and
not think about what he was doing down there - it is rather easy
when you can’t feel it. That had been something I was
worried about - having someone actually looking down there for a
period of time - the thought grossed me out - but it wasn’t
bad at all. I was able to laugh and joke and talk about Rocky
Mountain Oysters and other
odd foods (I was hungry - I hadn’t eaten since 9:30 a.m. the
previous day).
2:00 p.m. Still numb and cannot move to the wheelchair to be
moved to a maternity room. The nurses are very busy and cannot
clean me up to get me ready to move either so I have my husband
get me several damp washcloths, my under clothes, and
necessities. Then he left the room and I cleaned myself up. By
the time I am done with this, I can move a bit (only way to get
dressed) and call the nurse to take me to my new room. It’s
around 4:00 by now.
4:30 p.m. Am settled in my new room and they bring my wonderful
daughter. I have never been so happy and I keep crying with joy.
This is definitely worth everything! I would go through any of it
again for this conclusion. Am breast feeding and can feel the
contractions caused by this. Everything is as it should be. My dh
went home to bring back my daughter (another 100 mile round
trip). He should be back around 7 p.m. and will stay at Motel 6.
I will be released from the hospital on Saturday (it’s
Thursday).
NOTE: Was released on Saturday, but due to a blizzard was unable
to get home
until Monday.
Return to Birth
Stories
Return
to OPSS Main Page
The Birth of Caitlin Elizabeth
by Lisa Russell

Hope everyone had a wonderful
Thanksgiving! I know that in my
family we were all dabbing away tears of gratitude yesterday for
our
precious Caitlin Elizabeth. She was born on Thursday, November
20th
(11:59pm!) at 6 lbs, 4 oz and 19". Yes, I am very sore
(understatement, really), sleep deprived and still somewhat
disappointed with the negative hospital experience -- however, I
am
*deliriously* happy with my beautiful daughter. She was so worth
it
all. I find myself always studying her in rapturous wonder --
admiring her long fingers and toes (a future fashion model?), her
miniature version of my nose, her heart-shaped mouth, her dark
cap of
hair, her fathomless blue eyes and silver eyebrows (God almost
forgot
to give her a pair!) and taking in her special scent and soft
coos.
My blood pressure was up at my doctor's appt. on Monday the 17th,
so in addition to the usual NST and biophysical, I was sent to
the
hospital for monitoring. It was significantly lower there, so, to
my
relief, I was sent home. I had found out that day that my doctor
would be on vacation the week of Thanksgiving (the 22nd-29th),
and I
had a sneaking suspicion she wouldn't want to leave too many
patients
on her partner's hands & would use any excuse to have me fit
into her
scheduling. On the 19th I was proven correct. Dr. Fox had my BP
rechecked at her office and it had risen to 152/109 -- high for
her
to say "we're not fooling around with this anymore and
you're going
to the hospital to stay." I was in such shock (induction?
NOW?!) that
I didn't fight her on the issue, although it was obviously a case
of
medical convenience rather than necessity with Caitlin thriving
in
the womb. Despite the internal (only fingertip dilated and 0%
effaced) and my conviction that the baby would be overdue if it
were
up to her, I remained optimistic the induction would succeed.
Spent Wednesday afternoon hooked up the fetal monitor and BP
machine, with my BP slowly decreasing to the point that one nurse
said all the staff at the station were laughing at how mine was
better than all of theirs. Apparently, my doc had sent 6 patients
to
the small maternity ward, and the place was in chaos (BTW, this
wasn't the hospital for which I had preregistered, but I agreed
to go
there for my OB's sake). Spent a sweating, sleepless night on the
uncomfortable birthing bed with a dose of Cervicil inserted to
prep
my cervix, and at 5:30 am Thursday, my nutrition for the day
(saline/glucose IV) was hooked up. Minor contractions began at 6
am,
and the Pitocin was revved up a half hour later. Harder
contractions
began almost immediately, but very bearable and about 3 minutes
apart,
so all was well until about 11am when my doc's partner, Dr.D,
came
into break my waters. I was disappointed to only be at 2cm but
figured we still had a long while to go.
By midafternoon my uterus was hyperstimulated with back to back
contractions, and I was reduced to a pathetic, whimpering
creature
trying hard not to mangle John's hands and livelihood (he's a
medical
illustrator). Wasn't handling this pain stuff as well as I
thought,
and all the wiring (internal contraction monitor, internal fetal
monitor, catheter, IV, automatic BP cuff) wasn't helping matters.
When the doc announced I was still at 2 cm, I practically went
over
the edge and that's when my nurse suggested I take some Stadol.
Foolish girl, I agreed to the awful stuff, and for the next
several
hours was sent into a hazy curtain of confusion and pain. The
medication made my contrac's more irregular --e.g., doubles
followed
by a one minute break, triples followed by three -- but worst of
all
was how the drug would send me to sleep in between contractions.
John
said it was amazing how I'd be snoring for one minute (he even
videotaped it, the cad) & would wake for the next long,
painful
contraction, then go back to sleep.
I've never felt so out of control or just plain stupid in my
life. I know my OB came in at one point to ask when Dr. D has
given
me my last internal & I just couldn't answer her. I had lost
all
concept of time/place/people. The drug was finally wearing off by
the
time my last LD nurse, Sally (aka Nurse Hatchet), took over at 7
pm,
and I remember being soooo relieved to have my powers of
concentration back. Of course, the contrac's were still coming at
me
fast and hard, but my cervix never dilated beyond 2 cm (!).
Caitlin,
with all her mother's stubborness, was simply in no hurry to make
her
arrival & my body didn't want to cooperate with the evil
Pitocin. By
10 pm, shortly after another frustrating internal, I was sobbing
and
telling John I couldn't go on anymore and it wasn't long after
that
that Dr. D took pity upon me (and realizing the inevitable)
ordered
up an epidural.
Ah, the epidural. It was a horror getting in with Nurse Hatchet
practically laying across my head and shoulders while I tried to
remain still for 15 minutes with endless contractions and the
cuff
checking my BP. But it was so worth it and Dr. Brown is my hero.
My
BP immediately dropped too low and I was forced into various
positions & an oxygen mask, but Caitlin was never in any
danger and I
loved seeing those peaking contrac's on the monitor & not
being able
to feel them. Blessed relief. At 10:30, Dr. D came in and said
that
time was running out what with my waters having been broken and
we
could either go with the c-section immediately or wait. Feeling
cocky
due to the pain relief but knowing I was destined for the
operating
room (still only 2cm after more than 16 hours of labor), I asked
him
to wait an hour. In the meantime, I took smiling pictures, had
Mom
put some make-up on me (believe it or not) & prepared myself
psychologically.
I was wheeled in 11:30pm and the c-section ran like clockwork. I
was quite impressed by it all -- it was such a surreal
experience. Dr.
D didn't talk to me throughout the operation and it seemed like
forever before I heard Caitlin's first cry and another eternity
before they brought her to me. And boy, was she ticked! Guess she
was
counting on more time to do her hair and nails <g>. But she
was very
healthy, scoring 9/9 on the Apgars. I then was taken to recovery
until I could move my legs & then transferred to my room
where
Caitlin joined me around 7am. She took immediately to the breast,
but
in another disappointing blow, I developed a fever, was put on
antibiotics for two days & restricted from nursing. I started
up
again on Sunday morning, but the damage had been done. So my
daughter
and I began our running battles over the breast, which she
inevitably
always won -- filling formula in a no-work bottle was simply
preferable to her by that point. However, I did request an
electric
pump at the hospital to at first keep up my supply and then start
supplementing her with breast milk. My plan was to eventually
wean
her off the formula, but that isn't happening yet. Despite
remaining
wedded to the Medela Lactina I rented, my supply hasn't been able
to
keep up with her gluttonous demands; however, I'm grateful to be
doing something in way of giving her extra nutrients.
Recovery has been slow simply because I overdid it at first. The
old hospital only had full rooming in available (no nursery!), so
taking care of a newborn at night after Mom & John left was
horrendous and stressful. Just getting out of bed was a chore.
Check-
out time (Sunday afternoon) couldn't come soon enough for me,
although it would just be me and Caitlin on Monday &
thereafter. I
did all the no-nos: mopped, went to class Monday night, cleaned,
chased the dog down the street (couldn't let her be hit by a
car),
etc. until Tuesday night when my body punished me for my
Superwoman-
wannabe antics with major pains and strains. I'm now trying to
sleep
when Caitlin sleeps but it isn't easy with all the nervous energy
I
have. Anyway, time to pump again (feel like such a cow) and
admire my
darling baby girl. Best wishes to you all and I'll keep in touch
for
a while longer before signing off (isn't there a postpartum list
of
some sort?).
Return to Birth
Stories
Return
to OPSS Main Page
This site is hosted by Geocities
Home of the free webpage
"On The Wings Of
Love"
Courtesy of Jack's Shack
Design and Background by
Ashli
Gantt-Gillespie
©Copyright 1997